Health
- Details
- Health
Taking paracetamol makes us less empathetic towards others, according to a study carried out at Ohio State University. The results were published in the journal Social Cognitive and Affective Neuroscience.
During trials involving 80 college students, it was discovered that when participants who had taken paracetamol learned about the misfortunes of others, they thought these individuals experienced less pain and suffering, compared with those who had taken a placebo.
In the experiment, participants received four two-second blasts of white noise ranging from 75 to 105 decibels. They then rated the noise blasts on a scale of one (not unpleasant) to ten (extremely unpleasant).
They were asked to imagine how much pain the same noise blasts would cause in other study participants. The results showed that, compared to those who took the placebo, those on paracetamol rated the noise blasts as less unpleasant for themselves — and also for others.
‘Acetaminophen [the US brand name for paracetamol] reduced the pain they felt, but it also reduced their empathy for others who were experiencing the same noise blasts,’ the study’s co-author, Dominik Mischkowski, said.
A previous study by the same academics found that paracetamol also blunts positive emotions like joy. They say that, taken together, the research suggests that we need to learn more about one of the most common over-the-counter painkillers.
Baldwin Way, the study’s lead author, said: ‘We don’t know why acetaminophen is having these effects, but it is concerning.
‘Empathy is important. If you are having an argument with your spouse and you just took acetaminophen, this research suggests you might be less understanding of what you did to hurt your spouse’s feelings.’
Health News
- Details
- Elangwe Pauline
- Hits: 3934
- Details
- Health
Australian scientists have made a discovery that could lead to a simple and quick “breath test” for malaria. Researchers in the United States are developing a breath test for malaria, an innovation that could offer a cost effective alternative to blood tests. The breathalyzer test, still in its developmental phase, would be less expensive than current diagnostic tools such as a Malaria Rapid Diagnosis Test and wouldn't require blood samples or trained personnel to use it.
The CSIRO announced on Wednesday that a one million U.S dollar grant from the Bill & Melinda Gates Foundation will fast-track the testing, which will take place in a variety of climates and conditions around the world.
Over the next 18 months, a research team from the Commonwealth Scientific and Industrial Research Organisation (CSIRO) will undertake the field tests in a number of malaria-affected regions, including Malawi and Sudan in Africa, as well as in Bangladesh and the Malaysian province of Sabah.
Wednesday's news follows the discovery last year that distinctive chemicals can be detected in the breath of malaria-infected patients, making it quicker and easier to diagnose the disease.
On Wednesday, research group leader Dr Stephen Trowell said the funding generously given to the CSIRO by the Bill & Melinda Gates Foundation could eventually result in an 'over the counter' malaria test, which would allow for cheaper diagnoses and, in turn, cheaper treatments.
- Details
- Elangwe Pauline
- Hits: 3613
- Details
- Health
The Ebola scourge hit the shores of Sierra Leone almost two years ago when a man contracted the deadly virus in Kailahun, northeast of the country, in May 2014.
From there the disease spread like wild fire in the harmattan season, killing more than 3,000 Sierra Leoneans.
It also devastated the economy, and brought the country almost to a stand still.
Even though a number of victims survived the virus, they had to cope with mental wounds caused by it, and seek ways of healing.
Ericsson Turay, one of the survivors, conceived the idea to establish an Ebola Football team to serve as a meeting point for Ebola survivors in the community.
Eric told Xinhua in a recent interview that he himself contracted the disease when he was called to take care of some relatives who were suffering from the virus in Kenema, a city about 300 kilometres from the capital Freetown.
“With the help of the almighty together with medication, I was lucky to survive, but not so for 38 of my relatives who succumbed to the virus,” said Eric.
Left and abandoned to himself, Eric, with one of his friends, Nadia Wauguier, established the Kenema football team with other survivors with the aim of creating awareness of their plight in the county.
For now, he said, about 150 have registered for the club.
Eric said that the Ebola survivors live in loneliness abandoned by their community and despised by the government.
He said that if successful, the football team will help ease the physical and psychological pain most Ebola patients are going through.
They also intend to use the football team to reintegrate the survivors in the community.
CCTV
- Details
- Elangwe Pauline
- Hits: 3563
- Details
- Health
Chantal Biya, Cameroon's First Lady will be inaugurating this Friday at noon, the newly constructed Hospital of research and application in endoscopic surgery and Human Reproduction (Chracerh) at Ngousso district of Yaoundé, according to a statement from the civil cabinet.
Cameroon concord gathered that the foundation stone for the construction of the special hospital was laid back on the 1.12.1999. According to documents released to the press,the hospital, furnished with state-of-the-art equipment, is a specialised centre for the treatment of classic gynecology and obstetrics, outpatient, gynecological emergencies, cryoscopia, hysteroscopy , endoscopy, medical assistance for procreation, In vitro fertilization ,and the fight against infertility.
The hospital has 6 operating theaters, including 4 for gynecological surgery.The services of specialty doctors for emergency care are available throughout on all days of the week.
The hospital has ultra modern office space for doctors, as well as a cesarean section, a section for In vitro fertilization , numerous laboratories, delivery room, hospital rooms, a chapel, a mosque, a fitness and laundry room.
Hopefully this will convince government officials to go there for treatment rather than being evacuated to France as it has always been the case. Another question that plaques the common Cameroonian is,will the services of such an ultra-expensive hospital be available to the average citizen?
- Details
- Jackson Tantoh
- Hits: 6011
- Details
- Health
Millions struggle with tropical diseases causing blindness and other disabilities. DW talks to expert Martin Kollmann about getting vital drugs to the communities that need them the most - amid war, famine and unrest.
The Uniting to Combat NTDs coalition has published its annual report on the progress of the 2012 London Declaration on neglected tropical diseases (NDTs). Around the world, over a billion of the most vulnerable and disadvantaged people suffer from a range of NDTs. The global effort has focused on treating and eradicating 10 of them, including Chagas' diesease, trachoma, visceral leishmaniasis, leprosy and lymphatic filariasis.
DW: Professor Martin Kollmann, since 2012 there have been new efforts globally to fight, eradicate and also treat these diseases. Have much progress have we actually seen?
Martin Kollmann: I think we've seen fantastic progress since the London Declaration in 2012, when a very broad partnership of various stakeholders came together and made concrete pledges. The pharmaceutical sector pledged to donate drugs so that programs can become as cost effective as possible. We have the NGDOs, governments and funders coming together to make this happen and scale up efforts. And now we have a mechanism to actually track progress in a transparent way and hold each of the stakeholder groups accountable.
Could you give us some examples of where there's been progress?
Particularly in the area of lymphatic filariasis and onchocerciasis, preventative chemotherapy and the distribution of donated drugs that are free have been fantastic. In Latin America, river blindness for example is on its way out. There are just six indigenous communities in the Amazon border area between Brazil and Venezuela that still have this disease. And we have very good treatment coverage now in Africa. Keep in mind that we've impacted countries like the South Sudan, the Central African Republic and Congo. These countries have unrest, war, famine, huge populations, migration, and year after year we've been able to get those donated drugs to affected communities with the help of NGOs like the Christian Blind Mission (CBM) and others. Now we are in a position to actually have a paradigm shift moving from control of some diseases to elimination.
You've worked in Africa for many years - in Ethiopia, Kenya and many other countries. Can you give an example of what happens in a community where many people are affected by these diseases?
In river blindness you may have seen the image of a young child leading a blind father, mother, grandfather or grandmother on a stick. This child cannot go to school. As we prevent blindness in their parents and grandparents' generation, we actually give this child back a future. And if you go to these villages, in most parts of Africa you don't see new people going blind from river blindness anymore, and that is a fantastic success. But because the adult worm that produces the disease-causing baby worms live for many, many years, we need to deliver these drugs year after year. Despite war, famine and all the other catastrophes, the drugs need to be delivered to the entire community. And that has been done through this public-private partnership of health institutions in the most astonishingly successful way. That is why now these children have a chance to go to school - they have a future.
We've also seen whole villages that left their arable land around rivers where the black fly breeds - because they were "cursed" with blindness - can now go back and farm there again. So that's a typical example of the immense socio-economic impact that tackling NTDs can have.
Where do you see the biggest challenges?
Oh, there are huge challenges. We've made fantastic progress, but by far not enough. In 2015, we should have reached 75 percent coverage in treatment of all the population globally to achieve our goals. But we need better data, we have to know better where the disease is in the various countries, then we need to identify the barriers - why didn't we achieve everything we wanted to achieve, despite all this fantastic progress in the past year? And how do we overcome these barriers to become even more effective than we already are? These are not so much neglected diseases, but diseases affecting neglected people, the poorest of the poor living in areas with weak health systems. In many cases there is a dire need for more tools and more research. And there has been little investment in the past because these people don't have any economic power. They don't have a voice. Do you think in your lifetime you will see a complete elimination of these neglected tropical diseases?
I'm very optimistic. We are aiming to eliminate trachoma as a public health problem by the year 2020, and we are on track to do this. But we have to scale up our efforts. We need to do more, we need more funding, we need more research. Latin America shows us that it is achievable, as well as the progress that we've seen in Africa. But initiatives can only succeed if you work in a really open, transparent and close partnership with national programs and communities. So rebels may move in, and the drugs that are not distributed might be hidden in a hole in the backyard until the rebels have moved away. Then they'll be dug out and the distribution continues. We need to use whatever means available to get drugs out, year after year, to the people who need them most. This is not about charity. It is about empowering people and boosting local capacity.
Professor Martin Kollmann is part of the NTD NGDO network (NNN) and senior adviser on neglected diseases for CBM, the Christian Blind Mission in Nairobi, Kenya. Kollmann is a medical doctor and eye diseases specialist. He also teaches at the University of Nairobi's Institute of Tropical and Infectious dieseases and serves as Chair of the International Coalition for Trachoma Control (ICTC) and on the board of the German Network against NTDs.
This interview has been condensed for clarity.
DW
- Details
- Elangwe Pauline
- Hits: 3417
- Details
- Health
The Ministry of Public Health and a Canadian-based health technology company have signed a Memorandum of Understanding towards the creation of a mobile clinic.
According to the MoU signed this 27th April 2016, Cameroonians will receive technologically advanced and innovative healthcare services irrespective of their geographical location through the mobile clinic.
Public Health Minister, Andre Mama Fouda signed on behalf of Cameroon meanwhile the Chief Executive Officer of the Canadian company signed on behalf of his enterprise.
This mobile clinic will come to improve on health systems in the country and provide emergency medical assistance to patients.
A nurse practitioner, registered nurse and a primary care assistant will staff the mobile clinic to conduct regular checkups and treat minor ailments.
CRTV
- Details
- Elangwe Pauline
- Hits: 3799
Flourish Doctor Article Count: 3
Meet Your Coach Dr. Joyce Akwe ... With a master's in public health and a medical doctor specialized in internal medicine with a focus on hospital medicine.
Dr. Joyce Akwe is the Chief of Hospital Medicine at the Atlanta VA Health Care System (Atlanta VAHCS), an Associate Professor of Medicine at Emory University School of Medicine and an Adjunct Faculty with Morehouse School of Medicine in Atlanta GA.
After Medical school Dr. Akwe worked for the World Health Organization and then decided to go back to clinical medicine. She completed her internal medicine residency and chief resident year at Morehouse School of Medicine. After that, she joined the Atlanta Veterans VAHCS Hospital Medicine team and has been caring for our nation’s Veterans since then.
Dr. Akwe has built her career in service and leadership at the Atlanta VA HealthCare System, but her influence has extended beyond your work at the Atlanta VA, Emory University, and Morehouse School of Medicine. She has mentored multiple young physicians and continuous to do so. She has previously been recognized by the Chapter for her community service (2010), teaching (as recipient of the 2014 J Willis Hurst Outstanding Bedside Teaching Award), and for your inspirational leadership to younger physicians (as recipient of the 2018 Mark Silverman Award). The Walter J. Moore Leadership Award is another laudable milestone in your car
Dr. Akwe teaches medical students, interns and residents. She particularly enjoys bedside teaching and Quality improvement in Health care which is aimed at improving patient care. Dr. Akwe received the distinguished physician award from Emory University School of medicine and the Nanette Wenger Award for leadership. She has published multiple papers on health care topics.
Local News
- Details
- Society

Kribi II: Man Caught Allegedly Abusing Child
- News Team
- 14.Sep.2025
- Details
- Society

Back to School 2025/2026 – Spotlight on Bamenda & Nkambe
- News Team
- 08.Sep.2025
- Details
- Society

Cameroon 2025: From Kamto to Biya: Longue Longue’s political flip shocks supporters
- News Team
- 08.Sep.2025
- Details
- Society

Meiganga bus crash spotlights Cameroon’s road safety crisis
- News Team
- 05.Sep.2025
EditorialView all
- Details
- Editorial
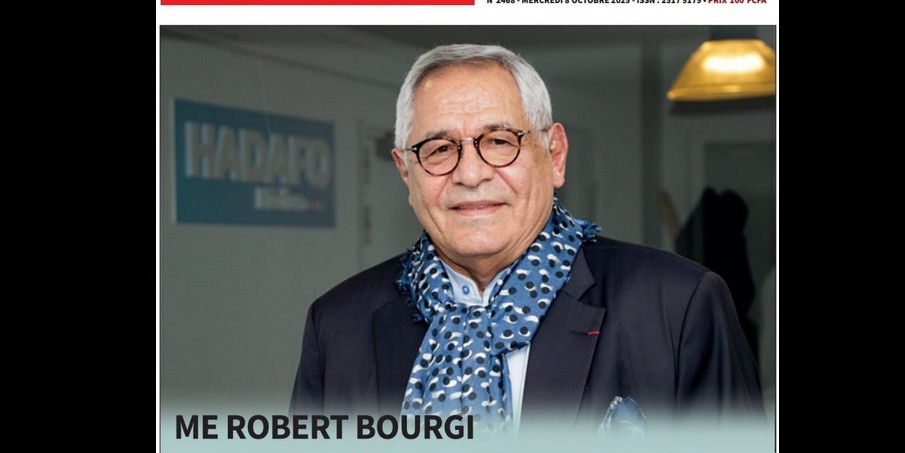
Robert Bourgi Turns on Paul Biya, Declares Him a Political Corpse
- News Team
- 10.Oct.2025
- Details
- Editorial

Heat in Maroua: What Biya’s Return Really Signals
- News Team
- 08.Oct.2025
- Details
- Editorial

Issa Tchiroma: Charles Mambo’s “Change Candidate” for Cameroon
- News Team
- 11.Sep.2025
- Details
- Editorial





